Download Tb Test Form in PDF
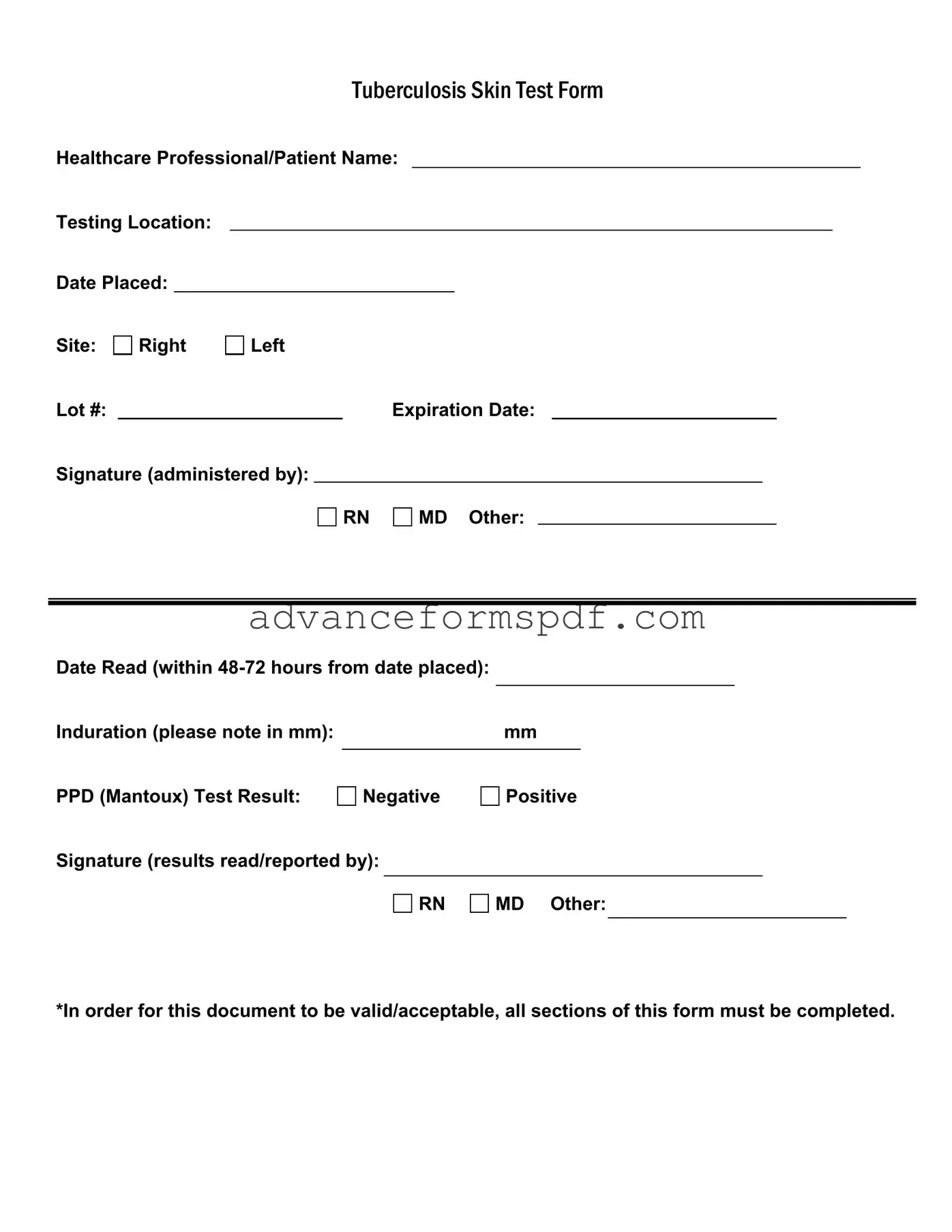
The Tuberculosis (TB) Skin Test Form is a crucial document used to record essential information related to TB testing. This form captures the healthcare professional's name, the patient's name, and the testing location, ensuring accurate identification of all parties involved. It includes specific details such as the date the test was placed, the site of the injection, and the lot number of the PPD solution, which is critical for tracking and quality assurance. Additionally, the form requires the expiration date of the PPD solution and the signature of the administering healthcare professional, whether a registered nurse (RN), medical doctor (MD), or other qualified personnel. Timeliness is vital, as the form mandates that the test be read within 48 to 72 hours from the date it was placed. The results, indicated by the measurement of induration in millimeters, are clearly documented, reflecting either a negative or positive outcome. Finally, the form must be signed again by the professional who reads and reports the results. To ensure validity, it is imperative that all sections of this form are completed accurately.
Document Data
| Fact Name | Description |
|---|---|
| Form Purpose | This form is used to document the results of a Tuberculosis skin test, commonly known as the PPD test. |
| Healthcare Professional | The form requires the name of the healthcare professional administering the test. |
| Testing Location | The specific location where the test is administered must be recorded on the form. |
| Date Placed | The date when the test is administered must be noted for accurate tracking. |
| Site of Injection | The form includes a section to indicate whether the injection was given in the right or left arm. |
| Lot Number | A lot number for the PPD solution is required for quality control and tracking purposes. |
| Expiration Date | The expiration date of the PPD solution must be recorded to ensure the test's validity. |
| Date Read | The test results must be read within 48-72 hours of administration, and this date must be documented. |
| Induration Measurement | The size of the induration (swelling) in millimeters must be measured and noted on the form. |
| Test Result | The result of the PPD test must be clearly indicated as either negative or positive. |
How to Write Tb Test
Once you have the TB Test form in front of you, it's important to fill it out completely and accurately. This ensures that the results are documented properly and can be used for your healthcare needs. Follow the steps below to complete the form correctly.
- Enter the healthcare professional's name: Write the name of the healthcare professional who administered the test.
- Fill in the patient’s name: Provide the full name of the patient receiving the test.
- Specify the testing location: Indicate where the test is being conducted.
- Record the date placed: Write the date when the test was administered.
- Identify the site: Mark whether the test was placed on the right or left arm.
- Lot number: Enter the lot number of the PPD (Mantoux) test used.
- Expiration date: Fill in the expiration date of the test material.
- Signature of the administrator: The healthcare professional who administered the test should sign here. Indicate their title (RN, MD, or Other).
- Date read: Write the date when the test results will be read, ensuring it falls within 48-72 hours from the date placed.
- Induration measurement: Measure the induration in millimeters (mm) and record the measurement.
- PPD Test result: Mark whether the result is negative or positive.
- Signature of results reader: The healthcare professional who reads the results must sign here and indicate their title (RN, MD, or Other).
After completing all sections of the form, double-check for accuracy. A fully filled-out form is crucial for it to be valid and acceptable. Make sure all necessary signatures are obtained to finalize the documentation.
Tb Test Example
|
|
|
|
|
TUBERCULOSISSKINTESTFORM |
||||||||
Healthcare Professional/Patient Name: |
|||||||||||||
Testing Location: |
|
|
|
|
|
|
|
|
|
|
|
||
Date Placed: |
|
|
|
|
|
|
|
|
|
|
|
|
|
Site: |
Right |
Left |
|
|
|
|
|
|
|
|
|||
Lot #: |
|
|
|
|
|
Expiration Date: |
|
|
|||||
Signature (administered by): |
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
RN |
|
MD Other: |
|
|
|
|||
Date Read (within |
|
|
|
|
|
|
|
Induration (please note in mm): |
|
mm |
|
PPD (Mantoux) Test Result: |
|
|
|
Negative |
Positive |
||
Signature (results read/reported by):
RN
MD Other:
*In order for this document to be valid/acceptable, all sections of this form must be completed.
Common PDF Documents
Puppy Health Record - Track your puppy’s developmental stages to ensure healthy growth.
Free Owner Operator Lease Agreement - Insurers are required to send relevant notices of coverage directly to the Carrier in compliance with regulations.
A Power of Attorney form in Arizona is a legal document that allows one person to act on behalf of another in financial or legal matters. This form is essential for ensuring that your wishes are honored when you cannot make decisions for yourself. For more information on how to obtain this important document, you can visit Arizona PDF Forms, which can provide peace of mind and security for you and your loved ones.
Affidavit of Custody - Notarization of the form ensures that the document is legally recognized.